Focus on Fibromyalgia and Depression: How Are They Related?

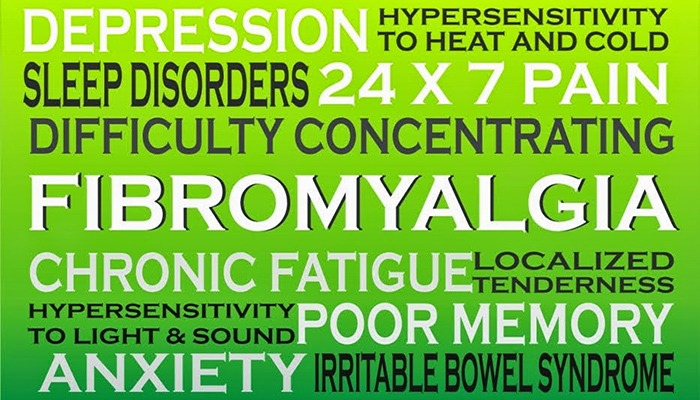
It’s not surprising that people with fibromyalgia often experience depression. Living with chronic pain and fatigue can create feelings of anxiety and loneliness. Many studies link fibromyalgia and depression. In fact, people with fibromyalgia are up to three times more likely to have depression at the time of their diagnosis than someone without fibromyalgia. But what is the link between the two and what can you do about it?
Who does fibromyalgia effect?
Research suggests that people with fibromyalgia are hypersensitive to stimuli that are not painful to others, perhaps due to a reduced blood flow to the portion of the brain that regulates pain. Additionally, Fibromyalgia appears to run in families, but scientists haven’t pinpointed a specific gene.
Fibromyalgia affects three to six million Americans – as many as one in 50. Women are significantly more likely to be diagnosed with the disorder and usually at childbearing age or older. And people with rheumatoid arthritis, lupus, and spinal arthritis are more likely to develop fibromyalgia.
How can fibromyalgia lead to depression?
Some researchers feel that depression leads to changes in brain chemistry. Others look at abnormalities of the sympathetic nervous system – the part of the nervous system that determines how you handle stress and emergencies. These abnormalities may lead to the release of substances that cause more sensitivity to pain. The result is fibromyalgia with chronic pain and feelings of depression.
What is the link between fibromyalgia and depression?
The stress from fibromyalgia’s pain and fatigue can cause anxiety and social isolation. The chronic deep muscle and tender point pain can also result in less activity. Coping with that pain and possibly people’s reaction to your condition can cause you to become more withdrawn from your “normal” life and can lead to depression. It is also possible that anxiety and depression are part of fibromyalgia, just like the pain.
“Depression and fibromyalgia often go hand in hand. But it’s the classic chicken-and-egg problem: What came first? Chronic pain, waking up feeling tired, having trouble sleeping, and other symptoms of fibromyalgia are pretty debilitating, and can often contribute to depression.” – Dr. Oz
Read how experts answer the question: “Is there a link between depression and fibromyalgia?”
How does stress play a role in fibromyalgia and depression?
The stress of living with chronic pain and persistent fatigue can make a person feel overwhelmed, nervous and anxious. What is unclear is whether a stressful life brings about fibromyalgia or if having fibromyalgia leads to stress. Either way, stress adds to problems of anger, distractibility, and irritability. Most people feel pain and fatigue increase when they have more stress. Sometimes, severe stress occurs just before the start of the disease.
How can you ease the symptoms of fibromyalgia and depression?
Depression and pain share the same roots in the brain and depression provokes pain, due to increased pain sensitivity. However both depression and fibromyalgia can be treated with anti-depressants. By following an appropriate treatment plan and getting the support of family and friends, you can take control of your fibromyalgia and symptoms of depression to improve your quality of life. Be sure to talk with your doctor.
Since depression and fibromyalgia can greatly interfere with your home and work life, it is important to openly discuss any symptoms of depression with your doctor. To understand your level of anxiety, take this online anxiety test.
For recommendations on living with Fibromyalgia, read our article: 10 Tips to Help You Cope with Fibromyalgia.
See medical expert answers to your questions in these Facebook chat transcripts: Fibromyalgia and Sleep and Fibromylagia and Chronic Pain.
Let us know your thoughts about fibromyalgia and depression. As always, we want to hear from you.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways