Radiofrequency Ablation – Is RFA for you?

Looking for minimally invasive pain relief without surgery? RFA may be the answer.
According to physician, Leonardo Kapural, Professor of Anesthesiology and Interventional Pain Physician, radiofrequency ablation or (RFA) is a medical procedure that uses radio waves to create localized electrical current. Such friction current makes a focused heat to target desired nerves. Interrupting the pain signal within the nerves can help to reduce chronic pain symptoms associated with various conditions.
How radiofrequency ablation works
“The ablation technique is semi-permanent. Interruption of pain signals may last until nerve regrows and nerve conduction re-establishes – typically 6-18 months,” says Dr. Kapural.
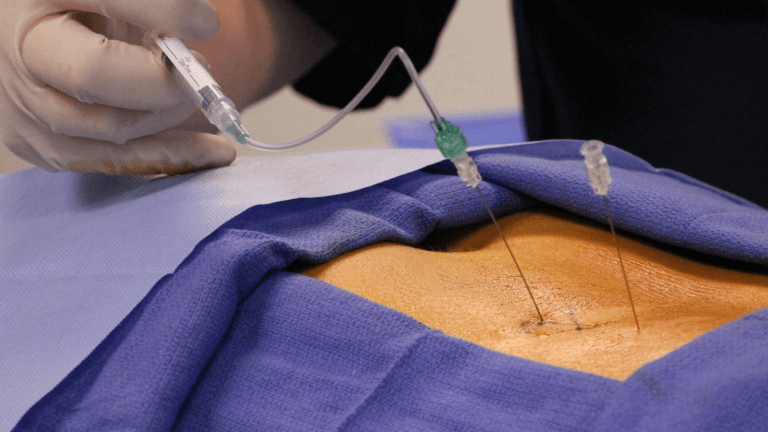
A physician uses a needle with a tip that heats up and places it very close to the nerve in the part of the body containing the pain. Through a process called thermocoagulation, the heat of the tip produces a controlled tissue destruction. Basically, with a radio frequency of 350,000 to 500,000 Hz, the heat causes the nerve proteins to coagulate and stop functioning. When they cease to function, the nerve can no longer send a signal to the brain that the area of the body is feeling pain.
Pain areas that RFA can treat
In patients with hip pain, RFA targets the articular branches of the femoral and obturator nerves. For patients with knee problems, RFA targets the genicular nerves. RFA is commonly used for knee and hip pain but also arthritis, neuropathy, lower back and even neck pain.
Dr. Kapural shares that recent advances in the use of RFA have allowed physicians to safely dramatically expand the painful areas of the body that can be treated.
“Nowadays we can denervate body painful areas from the head to toe. Recent studies documented long-term relief (8-12 months) from headaches, like severe migraines, cluster headaches, neck pain, thoracic spine and lumbar spine pain caused by advanced arthritis. Even for back pain origination from lumbar disc pain, there is a radiofrequency procedure called biacuplasty and for sacroiliac joint pain another one called Synergy. Finally, two new excellent indications for radiofrequency ablation are chronic knee and hip pain.”
Experts from Cleveland Clinic’s Department of Pain Management suggest radiofrequency ablation as an alternative to joint replacement when pain is the main motivation for treatment rather than joint instability. Functionality can be improved without the increased risk and complications of surgery. However, the experts do not think patients with all-over pain or severe fibromyalgia are good candidates for RFA.
RELATED: How joint protection can help prevent pain and injury
When RFA is commonly recommended
Dr. Kapural says that RFA is not considered the “last resort”. As an example, he shares that many of his patients who are not candidates for hip or knee replacement opt to have a 15-minute radiofrequency procedure that gives them about a year of profound pain relief. Those who are just too young, too old, too sick or just not ready for major surgery may receive hip or knee denervation.
“We believe earlier is better when it comes to treatment of chronic pain. In multiple studies, it has been shown that RFA can replace or reduce the amount of medications used for the treatment of chronic pain, including opioids,” says Dr. Kapural.
What to expect with the procedure
Physicians first conduct a test block before the RFA procedure to determine if future RFA would be successful. The diagnostic block utilizes numbing medicine (local anesthetic). If RFA is a good fit for a patient, it is frequently conducted using a small amount of sedating medicine and is minimally painful, as it involves only placement of thin RF needle to a specific target. The procedure is completed within 10-15 minutes, with the patient spending a short time in the recovery area and then discharged home. Recovery time is minimal or non-existent, as most patients would be able to mobilize with minimal pain same or next day.
In general, the risks with RFA are low and complications are rare. The most common side effects of radiofrequency ablation are swelling, bruising, and some mild discomfort at the injection site. However, all of the symptoms are temporary and will dissipate within a few days.
“Short-term irritation of the nerve, called neuritis, is possible (up to few weeks in few patients),” explains Dr. Kapural. “Damage to other nerves that may carry motor information is rare or non-existent, as those nerves are not targets of RFA. Infection or any bleeding would be extremely rare.”
Results patients should expect
Radiofrequency ablation – while very effective – is not permanent. Over time, the joint pain is likely to return once the lesioned nerves regrow. However, the good news is that RFA has been shown to be safe to administer repeatedly in patients with consistent pain reduction results.
Dr. Kapural says that expected pain relief will vary depending on the target chosen. In general, he expects that about 75% of the patients have more than 50% of pain relief at 6 months after the procedure and still more than 65% maintain the same relief at one year. Later than a year, pain relief dissipates and the procedure needs to be repeated. Functional capacity and a decreased use of medications use improves dramatically over the same time interval.
The future of RFA
Leonardo Kapural, MD, PhD
Physicians are becoming technically better in precise denervation that only nerves that transmit chronic pain. At the same time, they are able to expand the areas in the body where RFA can be used effectively, providing them with endless possibilities in stopping chronic pain of various sources.
“The next generation of precise waveforms and controlled lesion size will advance this procedure to a new level where we will be able to customize lesion size and shape and thus create a more predictable length of pain relief.”
Looking for a specialist for hip, knee or back pain who understands RFA? This website can get you pointed in the right direction.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways