Autoimmune & Pain CHAT 2016
What You Can Do to Live Better with an Autoimmune Illness
Transcript Highlights
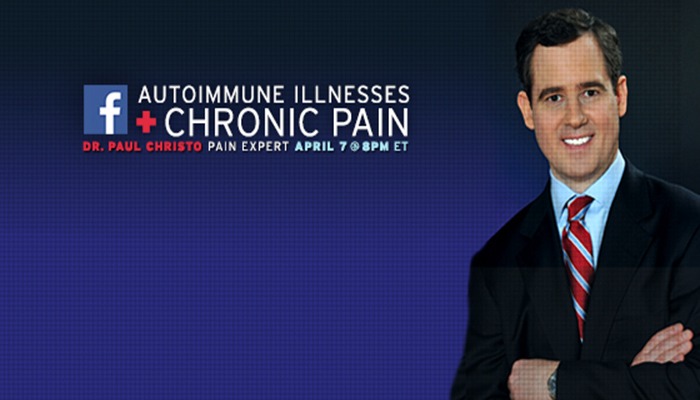
Dr. Paul Christo
April 7, 2016
Welcome! Thank you for joining us today for “What You Can Do to Live Better with an Autoimmune Illness.” This Facebook chat will be hosted by Dr. Paul Christo and will cover topics such as:
– Treatments (both medicinal and non-medicinal)
– The impact of diet and use of supplements
– Exercises that help (stretching, yoga, water aerobics, etc.)
– Alternative therapies, such as massage
– And much more.
Dr. Paul Christo is one of America’s leading pain experts and hosts Aches and Gains®, the first national radio talk show dedicated to overcoming pain, stress reduction, and healthy living. The show airs weekly on Sirius XM Radio, Family Talk 131.
He is also an associate professor, division of pain medicine at the Johns Hopkins University School of Medicine, specializing in treating patients with persistent pain in the spine, cancer pain, neuropathic pain, shingles pain, complex regional pain syndrome (RSD), post-surgical pain, and thoracic outlet syndrome. More details on Dr. Christo and his radio show can be found at www.paulchristomd.com.
Now, please join us in welcoming Dr. Christo!
Denise: Are there any new and/or successful treatments to help with the swelling/edema associated with CRPS/RSD?
Dr. Christo: Physical therapists can wrap the extremity in a compression garment, and sometimes diuretics are used if the edema is significant and doesn’t resolve with compression garments.
Dr. Christo: This was a good show on the connection between sleep and pain – take a listen.
Dr. Christo: Here’s another podcast that may be helpful, especially with so many CRPS/RSD folks on the chat tonight. File this away and take a listen to Not In My Head, when you have time.
Heather: Dr. Christo, do you feel diet plays a role in pain levels? Sometimes I can’t figure out what makes my pain levels spike at times. I have peripheral neuropathy, Sjogrens related.
Dr. Christo: Yes. I feel that foods that lead to inflammation can worsen pain. I tell my patients to limit fried foods, foods cooked at high temperatures, and animal proteins and substitute them for plant based foods, fish, and dark berries and cherries that can be anti-inflammatory.
PainPathways Magazine: Also, read our article on Food & Pain.
Kristina: I have a SCS with 4 leads that covers everything except my back and left arm. We will need to insert a 5th lead, under local anesthesia as I’m a very high risk for any surgery. I also use a 75 mcg Duragesic patch, Oxycodone 20 mg 3x/day and now lidocaine patches as well – to help control the pain. My pain management doctor is slowly titrating me down because of the current situation with opioids in this country; however, I can’t use ketamine (it almost killed me during my SCS surgery). I’m feeling backed into a corner because insurance doesn’t cover Calmare, LDN, etc. My pain management doctor is wonderful, but neither of us knows where to go from here. I have CRPS, full body now. Any suggestions?
Dr. Christo: I did forget to mention that Calmare therapy might be useful for CRPS. I would consider cognitive behavioral therapy for CRPS, full body. There are some inpatient programs in the country for pain. Johns Hopkins has one of these. You can call 410-955-8060 and ask for Brandie. I think it could help you.
PainPathways Magazine: Kristina, read more in our article on Advances in Neuromodulation
Beth: How can you find a good cognitive-behavioral therapist
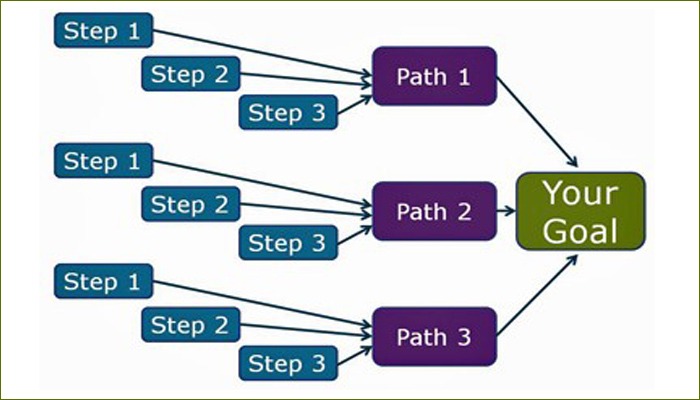
Dr. Christo: There are actually web based CBT programs today that are helpful. Patients can learn CBT techniques online, the states have a board of examiners in psychology, you can contact the American Pain Society or the International Association for the study of Pain, check out university programs in psychology, and pain specialists might also know of good therapists.
Dr. Christo: We did a two-part podcast on behavioral therapy that you all might also find very interesting and helpful. Here’s part one
Jane: Dr. Christo, can ECT help to manage chronic pain? I know it’s meant for chronic depressive type illness.
Dr. Christo: I’m not familiar with ECT as a treatment for pain. I’ve never recommended this to my patients.
Donna: I have a really bad case of fibromyalgia along with other issues and I don’t respond to regular meds that would normally treat it due to reactions. What changes do you recommend me to try? Pain is isolated worse to the trapezius muscle and SI joints. Thank you!
Dr. Christo: You could consider gentle exercise, actually. I’ve had patients benefit from swimming, light weights, and light cardiovascular work outs. Again, cognitive behavioral therapy can be helpful. A newer medicine called milnacipran (Savella) may help too.
PainPathways Magazine: You may also want to listen to this show on fibromyalgia. This guest was really great—she lives with fibromyalgia and has had struggles but also much success.
Beth: Can you explain Calmare therapy and how it’s different than using a TENS machine?
Dr. Christo: It uses skin electrodes to transmit a signal to the targeted nerve and systematically scrambles the pain response. It transmits low frequency electrical stimulation to pain receptors that in turn inhibit pain impulse transmission. It’s been studied in chemotherapy induced peripheral neuropathy, sciatica, low back pain, for instance.
PainPathways Magazine: Beth, this article on Calmare Therapy may help too.
Heather: Are there any new medicines or therapies coming soon to help chronic pain?
Dr. Christo: Yes. I think we’ll see:
- More abuse deterrent opioids for pain in generic form,
- New opioids that are designed to produce relief but have fewer side effects,
- Drugs that block calcium channels similar to pregabalin (Lyrica) for neuropathic pain,
- Drugs that block sodium channels that could be used for neuropathic pain in oral or topical form,
- Drugs that modulate something called the TRP channel to help with neuropathic pain,
- Cannabinoid (term used for all compounds structurally related to the psychoactive component in marijuana called, THC) receptor agonists (drugs like cannabidiol that reduce chronic pain and cancer pain). This is in the category of “medical marijuana”,
- Expanded use of botulinum toxin (botox).
Christina: Hyperbaric treatment, holistic therapy recommendations and medical marijuana, are these real options for treatment?
Dr. Christo: Hyperbaric treatment—I don’t believe there is much evidence on hyperbaric oxygen for autoimmune disease. However, a guest on the show I did on Lyme disease (Title: Ticks, Targets, and Terrific Pain), said that 72 consecutive days of this therapy for 2 hours each day was very helpful for her symptoms.
Dr. Christo: Marijuana—One research study on low dose THC and higher dose THC administered via a vaporizer showed significant pain relief in pain patients. Other studies have shown that smoked cannabis leads to reduced spasticity and pain in patients with multiple sclerosis. Another study showed that oral cannabis spray provides substantial relief in patients with neuropathic pain. A recent review article suggested that cannabinoids are safe and offer modest analgesic effect for chronic, non-cancer pain. I think that we don’t know enough about medical marijuana yet to determine its long term effectiveness or safety, but preliminary work points to its benefit.
PainPathways Magazine: On behalf of the magazine, we’d like to thank our expert and all those who participated in tonight’s chat! Be sure to join Dr. Christo on Sirius XM on Saturday as he talks with Diane Rehm!
We are excited to offer this great forum for information and inspiration.
Professional and individual subscriptions to
PainPathways Magazineare available at www.PainPathways Magazine.org.
All information provided is for educational purposes only. Neither PainPathways Magazine nor their Facebook Chat hosts are responsible for a medical diagnosis. Individuals should seek a physician for evaluation and personalized treatment plan.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways