Pain & Wellness Chat 2016
Pain & Wellness Chat 2016
Transcript Highlights
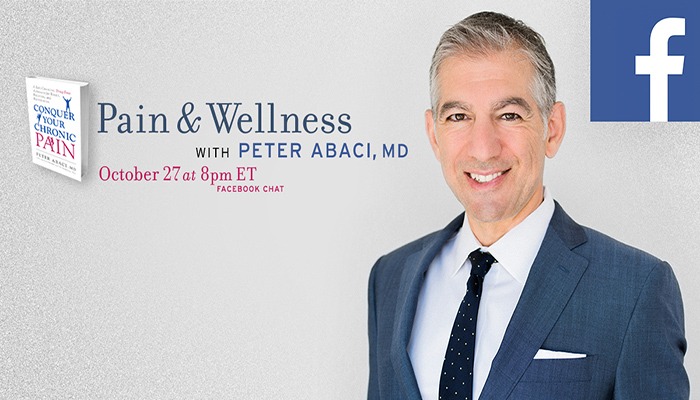
Dr. Peter Abaci
October 27, 2016
Welcome! Thank you for joining us today for “How to Manage Pain and Improve Life.” This Facebook chat will be hosted by Dr. Peter Abaci and will cover topics such as:
-tools to manage and heal your pain
-the importance of interdisciplinary care in treating CRPS
-tips on surviving changes in opioid policies
-tools to improve life with back pain/injuries
-advice for talking more effectively with your physician
-alternative therapies to get you on a path to wellness
PainPathways Magazine:
Peter Abaci, MD, is one of the world’s leading experts on pain and integrative medicine. His newly released book, Conquer Your Chronic Pain, A Life-Changing Drug-Free Approach for Relief, Recovery, and Restoration, is considered a must-read for anyone dealing with chronic pain.
Dr. Abaci, is certified in anesthesia and pain management by the American Board of Anesthesiology. Dr. Abaci received his undergraduate education at UC San Diego, where he graduated Magna Cum Laude and attended medical school at the University of Southern California. During his last year of residency, he served as chief resident and participated in a senior elective in pain management. That experience sparked an interest that led him to UC San Francisco, where he completed his fellowship training in pain management. In private practice since 1996, he serves as the medical director of the nationally recognized Bay Area Pain and Wellness Center, located in Los Gatos, California, which he cofounded with Dr. John Massey.
A widely respected expert on chronic pain management and a highly successful chronic pain sufferer, he is the author of Take Charge of Your Chronic Pain: The Latest Research, Cutting-Edge Tools, and Alternative Treatments for Feeling Better.
Dr. Abaci began his quest to radically change conventional chronic pain thinking and treatment after dealing with the agony of his second anterior cruciate ligament (ACL) tear. There is help for conquering chronic pain, without a life addicted to drugs, and hope for healing and long-term health. Commonly prescribed pain-killing medications—Vicodin, Demerol, Oxycontin, and other narcotics—can result in a heightened sensitivity to pain, along with addiction.
This has led Dr. Abaci to focus on developing alternative solutions to treating chronic pain. Drawing on neuroscience research, evidence-based medicine, ancient Eastern spiritual traditions, stress management techniques, nutrition principles, exercise programs, art therapy, and real-life lessons, Dr. Abaci focuses on creating an integrative pain-fighting regimen for his patients.
Now, please join us in welcoming Dr. Abaci!
Tammy: Been using Essential Oils for Pain relief with great success—any research updates?
Dr. Abaci: I would like to see more studies done on essential oils, as there has not been a lot published on their use. The mechanism of action remains unclear, and it would be helpful to have a better understanding of how they can work on the brain and the body. Some research suggests that their activation of the olfactory system results in feedback to emotional processing centers of the brain, like the amygdala. I am happy to hear that essential oils have played a valuable role in your pain management program, and I’m sure folks participating in our chat would be interested to know which ones you find therapeutic.
Melanie: How/what do you feel about patients using canibididiol (CBD) oil for pain? Do you think it works? What have been your experiences? Would you suggest it to someone before legal marijuana?
Dr. Abaci: I don’t have much direct experience with canibididiol oil, which some researchers believe has less in the way of psychoactive effects, and therefore more upside as a medicinal compound for treating pain and other ailments. How CBD and cannabis will fit into mainstream medicine is still an unfolding saga with lots of potential. As with any chemical or medication that you plan on using for an extended period of time, I always recommend caution when the long-term side effects are not yet well understood.
Becky:I have adhesive arachnoiditis from an epidural with depo-medrol, dura puncture. Multiple other chronic conditions. What do you recommend for neuro inflammation? Something that breaks the BBB.
Dr. Abaci: Arachnoiditis is a very challenging condition to treat, as I’m sure you can attest to! In general, when it comes to reducing nerve inflammation, many approaches may help, including following an anti-inflammatory diet (lots of produce with some healthy fats), stress-management techniques (meditation, yoga, breathing exercises), and improving the gut’s microflora with probiotics (yogurt, kefir, sourdough bread). The more healthy tools a person can acquire the better.
Sherry: Does he have chronic pain?
Dr. Abaci: As a matter of fact, I have struggled with two significant pain problems. One started with a knee injury in 2001, and the second, which was a pretty bad back/disc injury, occurred two years ago. If you check out the last chapter of my new book, “Conquer Your Chronic Pain,” you can read more about my struggles with my spine injury and how I have tried to overcome it. My own personal injuries and pain problems have had a big impact on how I approach my work as a physician.
Kimberly: What do you think of the daith piercing to help control chronic migraine pain? Also, any other treatments for people who have older rods used in scoliosis that are now not being used?
Dr. Abaci: I don’t have any direct experience using daith piercing for the treatment of migraines, but many of its advocates believe it works on pressure points much the way that acupuncture does. There seems to be some positive reviews of daith piercing on social media, but there are not yet any scientific studies to back that up. With any new treatment that comes out, I always stress looking at the safety profile very carefully.
Debbie: What do you think of the Calmar scrambler therapy for nerve pain. I’ve been doing it for almost 4 years. It helps but I still have flares of high pain in my hyst scar and no pain meds? The Calmar scrambler therapy uses electrodes to rewire the pain signals in the brain to help you feel no pain. It takes 10 sessions to start and then you get booster treatments for pain flares. It works for RSD, nerve pain and diabetic neuropathy. I’ve been doing it for four years and while I don’t get completely pain free it lessens my pain level and I’m off all pain meds. Dr. Stephen D’Amato is my doctor and he never gives up.
Dr. Abaci: Scrambler therapy is a relatively new treatment for pain, but there have been some positive studies published on using it over the last few years that sound encouraging. It sounds like it has been a valuable treatment for you, which is great to hear. For others reading this, I think it is worth considering if it is available and affordable.
Traci:What if any advances are being made in treatment of symptoms or in pain management? What is the future looking like?
Dr. Abaci: My opinion is that what really needs to change to conquer our pain epidemic is the way the insurance industry and Medicare approach the problem. Until that happens, doctors won’t have the best tools to truly help their patients at a deeper level, and by that, I mean providing the more comprehensive approaches that address all aspects of chronic pain including physical, psychological, social, vocational and even spiritual. Our healthcare system really needs to evolve in the way it approaches pain, and I’m hopeful that if we all speak loud enough, that it will happen.
Chelsie: How do you think we can decrease the opioid abuse, but still allow those patients who need the medication? I am 33, work full time, am a mother/wife, but have chronic pain that is controlled very well with opioids, but with new laws these medications are being taken away, and because of this my pain is no longer controlled.
Dr. Abaci: I think patients and their doctors need to start by asking the bigger-picture questions. Things like: How long do you plan to be on these medications? Do you want to be on them the rest of your life? What happens to patients who are on these medications for 5 years? 10 years? What are your long-term goals? Better quality of life? Becoming more active? Independence? Going back to work?
The answers to these questions help form the framework of developing a strategy between patient and doctor to move forward with. For example, if you are 33 and don’t want to be on your opioids in your 40s, then what else can be done to get you on the path you want to be? As I mentioned, our healthcare system has been too focused on just medications and there hasn’t been enough support for providing comprehensive integrated pain programs to patients. The more great care we can provide, the less we need to rely on opioids.
Tammy: I am wondering if there are any studies being done using PRP to help with nerve pains and other inflammatory processes.
Dr. Abaci: Most of the studies done on PRP (platelet-rich plasma) focus on treating injuries to tendons, ligaments, muscles, and joints. There have been a few studies published using PRP in treating peripheral nerve disorders, with some success, but not enough yet to really know where it fits in. I would imagine we will see more in the future.
Sue: How would you best advocate for fair, comprehensive pain management for those of us with multiple chronic pain sources? How would you suggest we advocate for humane and cost effective treatments? Let’s face it … no one with chronic pain would choose this! Thank you!
Dr. Abaci: As you may know, I help run one of the few true comprehensive interdisciplinary pain treatment centers in the country. The frustration and the tragedy here is that even though evidence-based medicine supports this model of care over pills and injections, most traditional insurance programs and Medicare don’t cover this type of approach.
As a result, most patients don’t get access to the type of treatment that may be what could help them the most. If federal organizations like the CDC and the Surgeon General want to come out so strongly against long-term opioids, then they should also come out even stronger for the healthy alternatives to help our patients get better. And I don’t just mean giving lip service, but really making insurance programs accountable for change.
The National Pain Strategy has a lot of very positive objectives in it, but how likely is it to come to fruition? I can’t really say.
One way that I have chosen to advocate for better quality care is by writing on the subject by publishing books, posting blogs, and participating in events like this. My hope is that what I write about will inspire the seeds for change at both a local level as well as at a national level. To learn more about my books, blogs, PainReliefRevolution.com, podcasts, and work for the Huffington Post and WebMD, please see my site: peterabaci.com.
Martyn:I spend quite a chunk on herbal anti-inflammatories and other supplements and vitamins each month, am I being taken as a suckered or do I really get the help that I think that I am getting?
I had progressed to needing a wheelchair to leave the house. I added turmeric three times a day and lots of B12, alpha lipoic acid, magnesium, DHEA and pregnenolone, both OTC potassium, boswellia and zinc. I also discovered meditation along with some basic yoga and I improved greatly, I started walking short distances and over a few months was up to three or four miles a day. I have arachnoiditis and cauda equina syndrome so I still need strong painkillers but I swear these supplements made the difference between existing and living.
Dr. Abaci: There is not a lot of scientific support for most of the vitamins and supplements that get used both for pain management purposes, as well as for other medical problems, but there are some reasonable options out there like alpha lipoic acid for nerve pain, fish oils for inflammation, and vitamin D supplementation when needed. If other lifestyle changes are not made, though, like healthy eating and good weight management along with exercise, then I think supplements are less likely to be effective. For example, for someone eating fast food, drinking soda, and smoking on a daily basis, I’m not sure there is any supplement that counteracts what this will do to the body.
Sandi: Are there any studies being done on how to turn off the signal that our brain perceives as pain? Also, any newer medications/treatments being developed? Lastly, there needs to be a treatment plan that doesn’t immediately tell us that we need to exercise, when some of us can barely shower.
Dr. Abaci: You might be interested to read about what I call the “Pain Brain” in my new book. Changing the pain message in our brains is a fascinating topic of interest for me. I discuss a lot of the research behind this and what types of approaches can be helpful in treating the “Pain Brain.” Everything from what we think, how we feel, how we breathe, and how we move all matter.
Certainly, there are a lot of new types of medications being studied. One category that I’m interested in following is the development of medications that can act specifically on glial cells in the brain. This is something that is still being researched but may turn out to be a product on the market someday. I appreciate the challenges and frustrations with exercise, but this is an area that I have done a lot of work. You may not have yet received the right help that you need, which is quite common in my experience. I have devoted a whole chapter in my new book to help with this.
Misty: Have you had success or helped anyone with interstitial cystitis? If so, I’m in to see if I can be free from this bladder pain
Dr. Abaci: To be honest, I have not seen a lot of success over the years with invasive treatments or medications. For the last few years I have worked with a physical therapist who specializes in treating pelvic floor problems like IC, and while it is not a magic cure, it can help address some of the muscle and soft tissue imbalances that can contribute to the pain. Along with that, learning relaxation techniques like biofeedback can also help. Acupuncture or transcutaneous electrical nerve stimulation may be helpful in some cases.
PainPathways Magazine: More info on IC:
Robin: I deal with migraine headaches with nausea almost weekly! What connection is there to the weather pressure and headaches during the changing of seasons?
Dr. Abaci: While weather changes seem to play a role in triggering migraines for some, including changes in barometric pressure, the reasons for this are still poorly understood as far as I know.
Debra:If RSD/CRPS has been around since the Civil War why don’t they teach about it ? I’ve been to doctors that have never heard of it and nurses that have no clue !!! They send you for physical therapy and they have heard of it so they end of making you worse. Why is it that the medical field won’t listen to the patients is it because they have a degree and I don’t ?? Why do I have to research and find a different doctor instead of my doctor doing the research ??
Dr. Abaci: I think you bring up a really good point. At this point, certainly at a minimum orthopedists, neurologists, pain specialists, and physical therapists should all be trained in how to recognize and appropriately treat CRPS. In our area, we offer PT students the ability to do rotations at my center, giving them a chance to see and treat CRPS for the first time, in many cases, but obviously that type of outreach is not nearly enough to make a difference.
April:What’s your view of inflammation and how to deal with it, through what kind of diet, vitamins and etc?
Dr. Abaci: I think inflammation happens in the body at many different levels. For example, there is the type you can see, as is the case with joint swelling, and what you don’t see in tissues like arteries, muscles, and nerves. Another interesting aspect of inflammation when it comes to chronic pain is over-excitation of glial cells, which has been a hot topic of pain research for the last several years.
I think there are many different ways of reducing inflammation inside the body. Certainly, good nutrition and an anti-inflammatory diet is a good start. I like to go by the rule of 7, meaning try to eat at least 7 different types of produce per day. Healthy fats from nuts, fish, olive oil and avocados are also important, but don’t forget to eliminate inflammatory foods from your diet like trans-fats and high glycemic foods. Get in the habit of reading labels and looking up glycemic index tables on the Internet.
Jennifer: I deal with chronic low back pain along with fibromyalgia. When I get a lot of pain in the SI and terrible sciatic pain, what can I do? I get epidurals but when they wear off it’s awful . My pain doctor refuses to give me pain meds—why I don’t know. Please give me some hope?
Dr. Abaci: I have also experienced some pretty intense sciatica, so I can relate to what that is like. One treatment that I have responded to is acupuncture. Sometimes it takes a few sessions before seeing results, but I know it doesn’t work for everyone. I also found that hanging from a pull-up bar can give quick relief by opening up the spine a bit. A good exercise and stretching program is also helpful, and I’m a big fan of Pilates for spine problems.
Dealing with sciatica at nighttime when you are trying to sleep can be the worst. I have used a combination of meditation, breathing exercises, gratitude journaling, and prayer to help me get back to sleep on those bad nights.
Shirley:What is your suggestion when you have been to every specialist you can think of and had every test imaginable, and still have no answers for your chronic pain except for an opioid prescription and a shake of the head, with a “Sorry, I don’t know,” when you ask what’s really wrong with you.
Dr. Abaci: Unfortunately, we don’t know everything in medicine, and we still have a lot to learn. That can be especially true when it comes to complex pain problems. But that doesn’t mean there isn’t a place for learning tools and strategies to help manage the pain. Here is a blog I wrote a few years ago on this very subject that you might find helpful.
More about opioids:
Shirley: Where (or to whom) do you turn when you feel like you’ve exhausted every avenue to try and find a treatment and solution to live a full life? How do you learn to trust doctors again when they treat you like an agenda and not their patient? I’ve officially given up after my last experience with a pain doctor and the neurologist he referred me to. All they both wanted to do was prescribe pill after pill that did absolutely nothing, and even after handing the neurologist a complete list of symptoms, she still dismissed me as having nothing more than sinus trouble (and then proceeded to push Botox and a super expensive migraine med on me). How do you find a doctor who looks at you as more than a cash cow?
Dr. Abaci: I think when it comes to treating complex chronic pain problems, a more holistic approach that treats the whole person is more effective. Another name for this is the biopsychosocial model, where in addition to looking at the physical disease side of the problem, doctors also look at the psychological and social aspects of the problem. This is why at my center we have a comprehensive team of clinicians including doctors, psychologists, physical therapists, art therapists, wellness instructors, acupuncturists, dentists, and nutritionists who all work together as a team for the good of the patient. All of these different perspectives can add value. If possible, look for a physician who shares this type of philosophy to help you find a more supportive team to work with.
Sara:What questions should one ask when interviewing and deciding on a pain management specialist? What qualifications should one look for?
Dr. Abaci: I think it is a good idea to be clear on what your goals are or what you want out of the relationship when choosing a pain specialist. Try to find a doctor who will help you with your goals and fits your philosophy.
Pain specialists can come from different backgrounds including anesthesia, physiatry, and neurology. Check to see what type of pain specialty training or fellowship has been done. Was it an accredited program? Look for board certification and if thier certification is recognized by the American Board of Medical Specialties.
Sharon: Pain not only affects the person suffering from it, it affects those we live as well as people we come in contact with. What the eyes cant see the mind cant comprehend so if we look well to the visible eye how can we make people understand how we are feeling and suffering on the inside.
Dr. Abaci: I appreciate the challenges in getting family and friends to understand what living with pain is like. Many patients that I first meet often feel very alone and isolated. But the reality is there are really an awful lot of others out there who are going through similar challenges. When they estimate that 100 million Americans are dealing with pain, they are talking about almost a third of the population. Once my patients start to meet and work with other patients with similar problems, they start to realize how many others are also struggling with pain issues.
One way of helping others understand is through education. Asking them to read a well put together book or article on the subject can be a good place to start. Sometimes it helps for them to get the information from an outside third party source.
Marsha: I got off opioids two years ago, after 13 years, and am attempting to manage my multiple chronic pain conditions with other methods. Every day, however, it seems like the balance changes: what worked yesterday doesn’t work today. Advice?
Dr. Abaci: First of all, coming off of opioids after 13 years is a huge accomplishment. Finding the right balance just might be an ever-evolving process where you have to continuously readjust what you are doing. Sometimes both our bodies and our brains respond to change and challenges more so than the status quo. My guess is the last few years have been a time for significant personal growth for you, and things are still coming together little by little. Take it one day at a time to avoid feeling too overwhelmed.
Donna: What would you consider the top medication free ways to deal with pain? Are massage, acupuncture, bio-feedback, etc. really worthwhile?
Dr. Abaci: There isn’t a one-size-fits-all way to treat pain. I think the main thing is to focus on getting healthy and well both inside and out as the way to put pain in its box. That can mean taking advantage of all sorts of modalities, especially the ones that empower you to be successful. For example, doing yoga has been really great for me when it comes to managing pain, improving my mood and decreasing stress, but that doesn’t mean it would do the exact same for you. I think there is a place for alternative treatments like massage, acupuncture, and biofeedback. In fact, things like tai chi, acupuncture and yoga have probably been around for centuries for a reason.
Kathy:Here’s one you probably can’t answer…..why did this happen to me?
Dr. Abaci: While I can’t answer this question literally, I do think this raises some things worth talking about. While pain, suffering, injury, and loss are all terrible things to deal with, there may be some silver linings in all of this to look for. Perhaps there is an opportunity for growth in all of this that you wouldn’t have had otherwise? Are there things that you have learned that could be helpful to others? Mother Teresa spoke of the call within the call, meaning dive deeper below the surface to find the true meaning and essence of purpose. I know this probably sounds heavy, but it is worth thinking about. I truly believe that my own injuries and pain challenges have made me a better doctor.
Donna Greyerbiehl: Are there good alternative treatments out there, that actually work AND that insurances are willing to cover? Insurance can play a big part in methods chosen.
Dr. Abaci: If you look at evidence-based recommendations for chronic pain treatment, you will see that the most effective type of treatment is the comprehensive integrated program where patients go through several hours of structured treatment and therapy on a daily basis for a number of weeks. This type of approach is also what I generally see to be the most impactful in my own practice.
The problem, as you point out, is this type of comprehensive care is usually not covered by most insurance plans. We need to continue to put pressure on the government and insurance industry to cover this level of care.
Insurance policies have served to drive an over-dependence on invasive procedures, surgeries, and medications for pain treatment which are often not the best choices for many.
Jackie Willis Carver: Are there any latest on neuropathy or RSD?
Dr. Abaci: I think CRPS is one of the most challenging problems in all of medicine to treat. In my experience and opinion, the more comprehensive the scope of treatment, the better the results will be. For example, just trying medications or just trying nerve blocks can only go so far. But when many different approaches are added together in a synergistic way, then I think patients respond better. It is important to treat the whole person, not just a specific nerve or injured body part.
PainPathways Magazine: Here is a great read about Paula Abdul’s battle with CRPS/RSD.
Cynthia Henderson Mittel: Do Spinal Cord Stimulators actually work?
Dr. Abaci: This is a topic where different physicians will have very different opinions. The technology on this seems to be still growing. Spinal cord stimulation is not my preferred method of providing long-term care to my patients. I think making a decision to go down that road should not be taken lightly by physicians and patients.
PainPathways Magazine: Informative article on SCS:
Tina Lamb: What kind of disease do you think fibro is? Autoimmune? Virus of some sort? Neurological? Central nervous system?
Dr. Abaci: Fibromyalgia is still in many ways a mystery. The immune system, neurologic system, and musculoskeletal systems may all have a role with this disease. I like to think of it as a state of central sensitization, where the whole system is extra sensitive to certain stimuli and pain. So, for me it is a central nervous system disease affected by many different factors in the body.
Jenny Isley Peery: So many of us feel hopeless, with our resources exhausted in the complex regional pain syndrome community. What kind of hope are you able to offer us?
Dr. Abaci: I meet a lot of patients with problems like CRPS who have come to feel hopeless but tell me that all changes once they hear about what can be done to help them function better and feel better. We happen to see a lot of patients with CRPS at my centers, and many of them make some pretty remarkable recoveries. It takes a lot of hard work and a team that understands how to work with something like CRPS to get results, along with a lot of patience and resilience. But absolutely I see great things happen to patients who are struggling with CRPS with the right level of care and guidance.
Now that doesn’t mean that the pain magically just disappears, but people can live a fulfilling and active life with this problem.
PainPathways Magazine: As a follow up to Jenny P.’s question, here is a great article on CRPS:
Cynthia John Toussaint-Garrett: Curious about how much emotional upset can flare us, Dr. Abaci… I got really upset while swimming at the YMCA yesterday, and afterward I suddenly had such sharp pain in my right leg, I still can’t put weight on it w/o screaming! It’s knife-like pain where I’ve been diagnosed with bursitis (and I’ve had body wide CRPS for 34 years). Also the weather just got cold and wet. I don’t understand HOW my pain can suddenly be this bad. Any thoughts or relief recommendations? ~ Cynthia Toussaint
Dr. Abaci: Cynthia, I always say that when it comes to pain, there are usually many layers to the onion. Our emotions can certainly impact the magnitude of our pain experience, and you can think of it as a volume control knob on the radio. Emotional distress can be like turning up the volume on the pain! So many of my patients get flared when the weather changes like this.
Pam Patridge: What do you think of using fentanyl for CRPS? Been on it over a decade now. Workers Comp says I can no longer have it. What do I do?
Dr. Abaci: Fentanyl is really the strongest opioid out there. It was originally invented to be used by anesthesiologists in the OR while giving anesthesia. Later, fentanyl versions came out to be used for terminal cancer patients who had developed a high tolerance to opioids. It really wasn’t intended to be used for more long-term chronic pain problems because of its potency and the risks associated with that.
Teresa Emerick: I have had fibromyalgia for 30 years and became extremely sensitive to chemicals. I use essential oils, massage, reiki, meditation, grounding, and some topicals to help manage it. As an integrative therapist, I now treat fibromyalgia patients with these same methods. Have you seen any recent developments that give clues to better management on the drug front? I have seen some improvements in states that legalized marijuana, but not everyone finds relief from it. Most of my patients that take meds seem to get worse, while those not on meds improve with integrative therapy.
Dr. Abaci: I have not yet seen a medication that consistently works well for fibromyalgia, and as you said, the side effects are often a problem. This is why a more holistic approach is often a good idea.
Michele Rice: What are your thoughts on Ketamine for RSD/CRPS? Any treatments that you have found to be helpful for myofascial pain in the jaw?
Dr. Abaci: Interest in ketamine has certainly continued to rise over the last few years. There are certainly CRPS patients that I have spoken with who believe in ketamine treatments, but it is not readily accessible to many. Another thing to think about is that we don’t really know what the long-term effects are with extended use. Ketamine is still in somewhat of an experimental stage but with promise for the future.
PainPathways Magazine: Great article on Ketamine:
Robin Scanlon Dorgan: I am a trigeminal neuralgia patient. My pain management doctor has recently told me that his practice is moving to a more interventional practice and moving away from long-term care, also they do not want to be involved with prescribing any benzos, antidepressants or sleep medications associated with chronic care. What advice to you have for pain patients whose practitioners are succombing to pressure and panic-driven legislation that seeming favor the addict instead of the patient?
Dr. Abaci: Robin, one of the tragedies of our traditional medical system is that it does not reward doctors for getting patients better or for creating good health and wellbeing. Instead, it rewards doctors for doing things. Part of the problem you are facing may be due to policy changes but part of it is also probably due to economic factors and how insurance companies reward doctors. This needs to change so patients get better care
PainPathways Magazine: More information on trigeminal neuralgia:
Cynthia John Toussaint-Garrett: Dr. Abaci, I’m interested in the studies that link childhood trauma to adult on-set high-impact pain. My father committed suicide when I was 8, and being the middle child and oldest girl I carried the burden of taking care of my four siblings. Do you subscribe to this connection? Thanks, Cynthia
Dr. Abaci: This is an important topic that more doctors and health care providers need to be aware of. Childhood experiences, including past traumas, seem to have a significant connection to chronic pain problems in adulthood. At my center, we always try to assess for factors like that. Chronic pain patients often need treatment for the activation of trauma-type symptoms as part of their recovery plan. I do touch on this a bit in my new book.
PainPathways Magazine: Everyone, our time is unfortunately up. We appreciate all of your thoughtful questions and our experts’ informative responses. Check back with us for our next Facebook chat!
PainPathways Magazine: Subscription discount! For a limited time, we are offering a one-year subscription to our magazine at $17. Enter coupon code: chat$17 at checkout. Order your subscription online.
PainPathways Magazine: Hi everyone! This is Amy North, editor of PainPathways Magazine. On behalf of the magazine, we’d like to thank our expert and all those who participated in tonight’s chat! We are excited to be offering this great forum for information and inspiration. We’ll post transcripts of the chat to our website soon. Have a good night everyone!
Professional and individual subscriptions to
PainPathways Magazine are available at www.PainPathways Magazine.org.
All information provided is for educational purposes only. Neither PainPathways Magazine nor their Facebook chat hosts are responsible for a medical diagnosis. Individuals should seek a physician for evaluation and personalized treatment plan.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways