Chronic Spinal Pain Chat 2016

Living with Chronic Spinal Pain Chat 2016
Transcript Highlights Dr. Anthony Berg
September 29, 2016
Welcome! Thank you for joining us today for “What You Can Do About Back and Neck Pain.” This Facebook chat will be hosted by Dr. Anthony Berg and will cover topics such as:
– Common causes of back and neck pain
– Non-surgical therapies that are available
– Other treatment options
– Advise for talking more effectively with your physician—How to get on a path to wellness.
As an anesthesiologist, Dr. Berg, a partner at Spine Team Texas, offers nonsurgical relief for acute and chronic spine pain. Dr. Berg completed his residency in anesthesiology at the University of Iowa and his fellowship in interventional pain management at Wake Forest University School of Medicine—Carolinas Pain Institute in Winston Salem, North Carolina.
As an offshoot of his clinical duties, he is a primary investigator on studies specifically looking at using spinal cord stimulation in the treatment of complex pain problems. Data collected from these studies have been presented and published numerous times further increasing our understanding of chronic back pain and advancing treatment options. In addition, Dr. Berg is the vice president of medical staff and medical director of palliative care at Presbyterian Hospital of Rockwall and is the medical director of the Texas Health Spine Surgery Center of Rockwall.
Now let’s welcome Dr. Berg!
Dr. Berg: First of all, I would like to welcome everyone to this live Facebook chat on the topic of chronic and acute spinal pain sponsored by PainPathways Magazine. As a point of reference I’m in anesthesiologist with subspecialty training in chronic pain and practice in a multispecialty group that focuses purely on spine pain. We are a team of neurosurgeons, orthopedic spine surgeons, anesthesiologists and physiatrists. For tonight our discussion will revolve around chronic spinal pain and how it affects patients. Questions are welcomed and hopefully we can have a good discussion.
Dr. Berg: As a point of logistics—so that I can offer as much opinion as possible—my responses are dictated through the computer which is much faster than typing, so there may be some transcriptional errors. I will try to catch those as best as possible, but if something slips through, please excuse it.
Dr. Berg: Also I should note, while I would love to be able to make recommendations for very specific cases, this can be very difficult in this forum. To fully evaluate a patient, a formal history should be taken, and examination should be performed, appropriate studies should be reviewed and at that point an impression and plan can be created.
Dr. Berg: With that, I’ll open it up for discussion. There were some people who have already sent in questions and we can start there.
Theresa: I’ve been trying to find research on stem cell therapy for cervical and thoracic spine areas but have only found info for the lumbar region. Are there studies being done for these areas and if not, why? It seems like all studies are done for the lumbar region. This happened with artificial disk and by the time it was approved for cervical most patients did not qualify due to a prior fusion. Why are there not more treatments developed for cervical/thoracic patients?
Dr. Berg: Theresa, you bring up a very good question. Certainly now there is a lot of attention regarding stem cell therapy and things like it. With regard to why it’s likely being trialed on lumbar areas versus cervical and thoracic areas, this most likely is due to the fact that the lumbar spine is safer to work in and is typically where a lot of the different therapies were trialed originally. Certainly, as efficacy is demonstrated in the lumbar area, often times these treatments are then carried up to the thoracic or cervical spine if appropriate.
Additionally, I would comment, I have often had patients with similar sentiments that no one can answer the questions in regard to a specific issue. One of the facts that I really have come to know is that when answers are very difficult to find, this is a hallmark feature of a very, very difficult question. While this seems very intuitive it actually means quite a bit. As an example, I’ve had patients come to me looking for a second opinion but when I realize that they have seen 6, 7, 8 or 9 doctors prior to me who have offered either the same solutions I’m offering or themselves do not know the best course of action It certainly reinforces that this patient’s case is very difficult with no clear solution.
Renee: I have a history of 12 spontaneous rib fractures. 10 out of the 12 fractures are posterior rib fractures. I’ve been to Riley Children’s Hospital, Mayo Clinic and Chicago…seeing experts, and they all tell me that I’m the only case with spontaneous rib fractures with no trauma. I’ve had extensive workup including lab tests, genetic testing, and imaging (x-ray, CT, MRI, bone scan, and dexa). Around 4 of my rib fractures were displaced (the ends of the broken ribs were approx. 1.5 inches apart from each other) and healed that way (they did not come back into alignment). I still have significant/debilitating pain in the ribs that healed displaced. This is even after 8 years since the initial fractures. I do not experience pain anymore for those that healed located. MY QUESTION: What else, if anything is there left for me to maybe try that you think might help with my chronic rib pain, especially the raw bone pain?
Dr. Berg: Renee, you certainly have a challenging case here. Definitely through you history it can be seen that you have tried multiple opinions as well as quite a few very respectable places. With a condition that is so rare the recommendations that can be made are oftentimes based on educated guesses. It certainly seems that these physicians have tried just about everything that is out there for the treatment of pain with the exception of the pain pump which you mentioned in your for question. Admittedly I have little experience in regard to chronic rib pain as my practice focuses solely on pain of the spine. What I can say is that it appears that the physicians you work with are really trying to help you out in what appears to be a very concerted effort.
PainPathways Magazine: Bookmark this site – this is where Dr. Berg works and the site has great resources to check out.
Keith: Dealing with SCS technology…what do you foresee as the next big step with this type of treatment? I have researched the current mfg and understand 60Hz technology compared to 10kHz technology.
Dr. Berg: Mr. Armstrong, spinal cord stimulation right now is evolving rapidly. As you mentioned, one of the current areas of research is in the frequency in which electricity is transmitted to the spinal cord. There are certainly many studies going on right now looking at different frequencies such as conventional rates, rates around 1000 Hz, 10,000 Hz and even higher. With so much effort being placed in this avenue of investigation as data begins to pour out of this, I think we’ll have a better understanding of what rate or waveform may be best for the treatment of different types of chronic pain. It’s very important that patients participate in the studies if at all possible. Unfortunately we do not know currently what the best rate or waveform is, but I do feel confident that in the near future this may become more of reality.
Other issues regarding spinal cord stimulation are making more systems conditional for MRI scanners, miniturization as well as decreasing of common complications such as migration of the leads used in stimulation. I also see improvement in patients’ interactions with their devices so that they can control the device in a better way, offering better pain control. I also know that newer interface technologies to allow distance programming and troubleshooting are being explored.
PainPathways Magazine: As a follow up to Keith’s question, here is a helpful article for folks considering SCS:
Sandra: I have been diagnosed with degenerative disc disease and I’m only 30, what treatments would you suggests to help slow this disease?
Dr. Berg: Sandra, without knowing the specifics in the degree of your degenerative disc disease, I would probably offer these recommendations in a very general sense. First, it must be understood that degeneration of disks is a natural process that occurs over time. Oftentimes, patients will come to me being told they have degenerative disc disease and are somewhat frustrated and scared. As they are educated, they understand that this is a natural process of aging. Certainly there are cases where people who were fairly young have more advanced degeneration and that may be from specific catalyst in earlier parts of their lives.
In general, however, our biggest recommendations revolve around a few different issues. First, any patient that is smoking, it is of utmost importance that they stop smoking as this contributes significantly to quicken degeneration of disks. Second, encouraging patients to exercise more and live a healthy lifestyle. Thirdly, carrying excessive weight or being overly sedentary certainly can contribute to disks degenerating faster over time. Additionally, I encouraged patients just to live a healthy life to the best of their ability, which can certainly decrease the rate of decline.
I strongly believe that if the patient is beginning to have symptoms of back pain it is imperative that patients meet with a physical therapist and learned the proper exercises and troubles to strengthen their backs and improved their cores.
PainPathways Magazine: At all of our chats, people often ask this question, and here is some advice from our website that may help.
Monica: I have sciatica, what are steroid shots? How will they work?
Dr. Berg: Monica, sciatica is another term for radiculopathy. This term refers to the fact that the nerve root of the sciatic nerve has become irritated. This is most often seen with an acute herniated disc, disc extrusion, annular tear or a bone spur pressing up against the nerve root. Symptoms that develop from these pathologies include pain not only in the back, but going down the leg in a very specific pattern depending on which nerve root is being irritated.
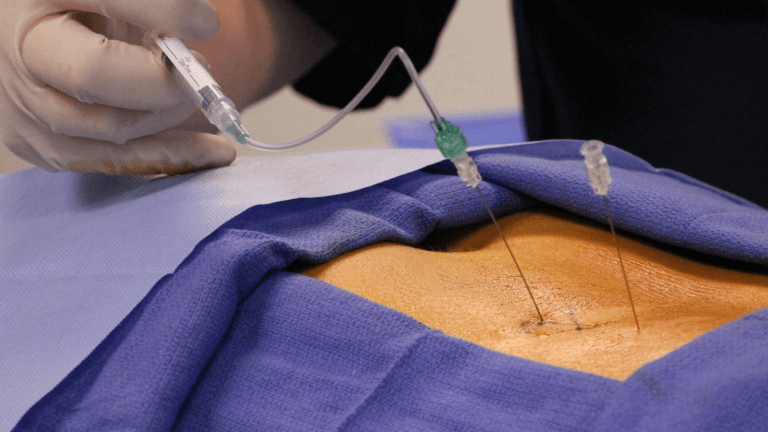
With regard to steroid shots, more commonly called an epidural steroid injections, these procedures are utilized to decrease the inflammation around the nerve root therefore decreasing the pain that a person may experience.
For the physician they’re also an excellent diagnostic tool in understanding how a person responds and what other treatment options may be necessary. For instance, if pathology is seen clearly on an MRI demonstrating compression of a nerve root and the patient fails to respond to epidural steroid injections, it may be considered that this person might need to have a surgical intervention. In this way we can approach a person’s case in a lateral-like fashion using the least aggressive and least invasive approach and moving toward more aggressive therapies as they are appropriately indicated.
Keith: Are there evidence-based studies that show the success rates during the trial period? If so, what are the best resources to explore these studies? I do realize that each patient is different, but I’m trying to be as informed a patient as possible.
Dr. Berg: Mr. Armstrong, as a follow-up to your question regarding spinal cord stimulation I can appreciate you trying to be as informed as possible. To my knowledge there are no significant evidence-based studies that show success rates during the trial period of the spinal cord stimulator.
To help the audience understand spinal cord stimulation, this is a therapy where small wires are placed within the spinal canal over very specific part of the spinal cord. What is unique about this therapy is that unlike other interventions such as surgery, when a patient is being contemplated for spinal cord stimulation, a trial is done and these leads are placed for approximately a week. During that time the patient can utilize the device to see how well he can control his pain, and then when they meet back with the physician they can determine if this is a therapy that they would like to pursue in a more permanent fashion.
It’s my opinion that success rates during trial revolve around the actual diagnosis being treated, the technical ability of the physician, as well as the proper choice of the device being utilized for the treatment of their chronic pain.
Donna: I injured my SI Joint in a fall, 4 years ago, and still it gets incredibly painful.
Have done PT, TENS unit, injections at the pain clinic, etc. PT said when it is at its worst my pelvic seems to slip out of alignment. Any permanent options to take care of this or other options for it to keep from becoming so interruptive?
Dr. Berg: Donna, SI joint pain can be particularly painful, as I have experienced this myself, so I can offer some empathy. While I can’t offer a specific opinion on your case, as I don’t know exact features, there are some new options regarding SI joint pain. There are companies that are now offering minimally invasive fusions of the sacroiliac joint. This is typically an outpatient procedure and I certainly have seen success for those patients that have had chronic sacroiliac pain. Additionally, while you mentioned injections into this SI joint, another modality of treatment may be a radiofrequency ablation of the sacroiliac joint.
PainPathways Magazine: With so many folks interested in neuromodulation, this article may be helpful.
Keith: What could be some of the causes of a term that I’ve heard called “failed back surgery syndrome”? Is that an actual term?
Dr. Berg: Failed back surgery syndrome essentially refers to people that have had back surgery and to some degree it has not been effective in controlling the person’s pain. For example, a common scenario would be a person who had back pain going down her leg and had surgery one or more times but continues to have persistent symptoms. Hence, the back surgery has failed. Sometimes also called post laminectomy syndrome.
PainPathways Magazine: While osteoarthritis hasn’t come up specifically tonight, we get a lot of questions in general about this condition and chronic back pain.
Darlene: I recently had x-rays on my neck as my neck cracks with every movement. The X-rays show that I have a degenerating spine. I would like to have some suggestions for help. I am not in pain but it is stressful just doing ordinary tasks with constant cracking inside my head. I have been dealing with this for five weeks now. I also suffer from fibromyalgia and take 300mg of tramadol daily, which really has helped me to function.
Dr. Berg: Darlene, you bring up a comment that I hear my office quite often. Patients will complain of hearing popping sensation or grinding sensation in their necks and are concerned about that. Simply put, this is likely the physical manifestation of degenerative changes of the spine. The reason that you hear this so much is the mere fact that you ears are attached to your head and I suspect that if your ears were attached other parts of your body you would hear knees crack, hips grind and similar.
While this can be somewhat disconcerting, for the most part this is more of a nuisance. Certainly if this is a new symptom or has never been present especially if after a traumatic episode or some specific incident, it’s likely that this should be evaluated by a physician.
Likely a first course of action would be to have your physician prescribe something like physical therapy where they can work on mobility and strengthening of the neck. Range of motion exercises would be particularly beneficial with some of these clinical symptoms.
Chelsie: Hello there- I am 33; I have EDS type 3, a spinal cord tumor (at T12), a herniated disc (L1), and degenerative disc disease. I’m in pain all day, everyday despite being on opioid pain meds, and having steroid injections. Have you known spinal cord stimulation to work on patients with this widespread of pain? Are there any supplements you know of that works for this level of pain? Thank you!
Dr. Berg: Chelsie, spinal cord stimulation can be very effective in treating people’s pain. First and foremost, it is most effective in treating neuropathic pain. So it would be important in your case to know exactly what is causing what elements of your pain picture. This can often help the pain physician understand if spinal cord stimulation may be a modality for you or not.
With regard to supplements, I utilize a physician in the area who specializes in this, so I have little experience.
Kelly: I am concerned about the meds used to treat facet joint pain, and I have spinal stenosis in both my neck and lumbar spine. Does it cause the cartilage to break down? Do you have any other suggestions on pain relief for this type of problem? Thank you.
Dr. Berg: Kelly, being concerned about the medication used in your injections is very reasonable. Probably the biggest issue with injections is that we typically and most frequently used steroids. Certainly over time steroids can have deleterious effects. You should work with your physician to make sure that you’re not receiving too much steroid over time.
An alternative to receiving facet injections over and over is to have a radiofrequency ablation, which typically will offer more long-lasting benefit without the deleterious effects of the steroids.
Donna: I have spasticity from a stroke w/ L hemiparesis, 10 years ago, plus spastic torticollis, also due to my stroke. It goes from my neck, on left side, down to my L shoulder blade.
We do some Botox injections, plus trigger point injections, which help. But, was told not to use TENS machine near my neck? Why?
Dr. Berg: Donna, My recommendation if you have significant spasticity from stroke is to work with the physiatrist who specializes in spinal cord or brain injury. Often times they have better techniques for treating this. Unfortunately I do not treat any patients with post stroke hemiparesis or pain. With regard to the TENS unit I think this is more of a safety issue because there are certainly some nerves that run close to the surface of the skin, which, if stimulated, may cause some untoward side effects.
Donna: I know osteoarthritis is considered wear and tear arthritis, but can there also be an inflammatory component to it?
Dr. Berg: Donna, arthritis actually means “inflammation of.” All types of arthritis have an inflammatory component. That is why anti-inflammatories are so great when appropriate in arthritis-type conditions.
Chris: I have 3 herniated discs in my neck c3 c4, c4 c5, c5 c6 I think and degenerative disc disease. I have been told by different doctors that I’m not a candidate for surgery due to my age and both things going on with my neck. I didn’t respond to PT, I had ESIs and nerve blocks with little to no effect. I have even tried chiropractors. I think they may have made the pain worse. Pain meds help take the edge off but I don’t want to be completely dependent on them. I would rather not take them. What other options are there so I can function throughout the day and not be in pain the next.
Dr. Berg: Chris, You have a common scenario seen in the clinic: multiple levels of pathology with few surgical options. These options may be limited because of things you mention such as age, comorbidities, as well as complexity of the problem. It sounds like you’ve done the right things in regard to trying physical therapy as well as injections and nerve blocks, but unfortunately you’ve had little benefit. I completely understand your view on pain medications and not wanting to become dependent on them.
There are medications, however, that can help with pain that do not cause dependenc, and I think you should discuss that with your physician.
In my experience, when the patient comes in with certain expectations and realistic parameters in which they want to be treated, I am totally on board with trying to accommodate those, especially when those parameters are good for the patient’s health. Have this discussion with your physician. I think you may find it helpful.
Chelsie: Not sure if I can ask multiple questions, but here is another one. What is your opinion on the new laws regarding restrictions of opioid pain medications for chronic pain patients? I am currently being negatively affected by these laws, being that my pain management doctor is retiring, and has to take me off all my medications before I do so, and a new pain doc cannot get me in for several months. So, I suffer, without my medications, for months, because of these laws.
Dr. Berg: Chelsie, as you have personally experienced, the laws and regulations regarding opiate pain medication have certainly been a hot topic in the management of chronic pain. Specifically, in different states there are different regulations about who can manage chronic opiate medication. This has certainly caused an access issue in different locales.
I think I have mixed opinions regarding these laws. I can certainly see the benefit for the public in regard to the fact that decreasing access to those that should not be receiving those medications. However, just like most things, this has a negative impact upon people who rely upon these medications to function a normal life. I think, as this becomes a more prevalent issue, hopefully the side effects of change will be realized and steps can be taken to mitigate those.
Keith: If you have time to answer my previous follow-up question about repeating RFA in the written transcript, I will read later. Thank you so much for doing this session tonight!
Dr. Berg: In general, if people responded to RFA in the past and they had a good benefit, it would be my opinion that this should be repeated, especially if they’re getting long-standing benefit. It’s a fairly low risk procedure and only if it did not offer any benefit into the future would I move on to a more aggressive treatment option.
Dr. Berg: It was great to chat with this online community in this format with patients and people who have concerns regarding chronic spinal pain. Certainly there are many cases that can be very challenging while some may be more straightforward. It’s my hope that each patient who suffers from chronic pain may be able to utilize this as a resource as well as other resources to help improve their situation and their quality of life.
PainPathways Magazine: Everyone, our time is unfortunately up. We appreciate all of your thoughtful questions and our expert’s informative responses. Check back with us for our next Facebook chat!
PainPathways Magazine: Hi everyone! This is Amy North, editor of PainPathways Magazine. On behalf of the magazine, we’d like to thank our expert and all those who participated in tonight’s chat! We are excited to be offering this great forum for information and inspiration. We’ll post transcripts of the chat to our website soon. Have a good night everyone!
Professional and individual subscriptions to
PainPathways Magazine are available at www.PainPathways Magazine.org.
All information provided is for educational purposes only. Neither PainPathways Magazine nor their Facebook Chat hosts are responsible for a medical diagnosis. Individuals should seek a physician for evaluation and personalized treatment plan.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways