Michael Finkelstein, MD
Michael Finkelstein, MD, encourages patients to take the slow approach to good health. It’s not always easy, but it can alleviate a host of ills.
Michael Finkelstein, MD, the “Slow Medicine Doctor®,” says his slow approach to wellness is right for everyone and every condition.
“Every condition?” I ask him. (I’m a skeptic.)
“Yes,” he assures me. “Therapies are like seeds you put into the soil. If the soil isn’t ready for that seed, the seed is not going to thrive. Slow medicine is like cultivating healthy soil. It can mitigate and even alleviate a lot of conditions.” Dr. Finkelstein is a gardener, so it’s natural for him to use the garden as a metaphor.
I ask him: So, what about people who are eating healthfully, exercising regularly, managing their stress and still have a chronic condition?
“That’s exactly the person who comes to me,” he says. “My patients are often doing all the right things but still struggling. People often say to me—and they believe it themselves—‘I’m doing everything I can,’ but they’re usually missing something. There’s something out of balance.”
If you’re imagining Dr. Finkelstein as a hippie who practices his brand of medicine out of a yurt, forget it. The doctor earned his undergraduate and medical degrees from the Ivy League University of Pennsylvania, where he graduated Phi Beta Kappa and summa cum laude.
He’s as establishment as they come. Or, he was. Until 9/11.
slow medicine The Day That Changed Everything
In 2001, Dr. Finkelstein was medical director at Northern Westchester Hospital, 45 minutes outside New York City. As he and the staff watched the second terrorist attack on live TV—and saw the aftermath—they wondered what they could do. “As health care professionals, we felt helpless,” he says. Virtually everyone was looking for a way during that surreal time to be of service.
“That day, someone from the community brought the hospital a check for $1 million,” he recalls. “He said, ‘We need an integrative medicine center here. Here’s the money to get it started. This was at a time when most people didn’t know what ‘integrative medicine’ meant—when alternative medicine wasn’t considered credible. But as the medical director, it was my job to get educated and start this center.”
So, the doctor who thought his career path was set went back to school at age 40 to learn integrative medicine. Just as he had in undergrad and med school, he again sought the best teachers. He enrolled at the University of Arizona College of Medicine, where he completed an associate fellowship in integrative medicine, studying directly with—perhaps you’ve heard of him —Dr. Andrew Weil.
Dr. Finkelstein returned to New York and ran Northern Westchester Hospital’s integrative medicine program for three years, but when the funding ran out, the hospital chose not to continue the practice. But Dr. Finkelstein had seen how what he came to call “slow medicine” benefitted people with conditions from the mundane to the potentially life-threatening.
Treating the whole person, he found, simply leads to better outcomes.
He was already such a believer, he couldn’t go back to strictly conventional medicine. He opened his own Westchester, New York, center for integrative health, SunRaven, and became the Slow Medicine Doctor, executive director of The Slow Medicine Foundation and, in 2015, he published Slow Medicine: Hope and Healing for Chronic Illness, which was endorsed by both his mentor, Dr. Weil, and another well-known believer in integrative medicine, Mehmet Oz, MD.
Our Blind Spot
Dr. Finkelstein believes the clue to what’s missing is already inside us. We just need to dig.
“There’s usually one essential thing people are not doing,” he says. “We all have a personal history of [emotional] trauma and imbalance that impacts us physically. And we all have a blind spot.”
Dr. Finkelstein helps his patients find that blind spot. And it can be difficult, deeply personal work.
He developed 77 questions that he asks patients to ponder. (He also wrote a 2013 book about those questions and DIY guide on how to use the answers called 77 Questions for Skillful Living: A New Path to Extraordinary Health.)
“When I ask my patients these questions, there is often one—sometimes several—that they find upsetting. ‘Are you happy with your sex life?’ ‘What’s your relationship with your parents like?’ ‘Do you spend time outside?’ We’ve all been hurt in life. The body can have an inflammatory response to that pain. If your sister calls you out on this stuff, you scream at her. Well, that’s because it means something. It hits close to home.”
The questions, he says, often lead to a “sentinel moment”—a catalyst that can bring about change. When you dig deep (there’s the garden analogy again), you can make profound discoveries.
Of course, there can be emotional pain associated with these “aha moments.” About half of Dr. Finkelstein’s patients spontaneously begin crying when they get to that question that unlocks the source of their pain. Dr. Finkelstein is ready to help.
But, if he feels long-term counseling is needed, he’ll refer patients to a therapist. Here is where his training in integrative medicine comes into play. He says, “I tend not to send people to conventional practitioners. I look for people who are holistic, psycho-spiritual counselors. I want someone who understands the body/mind connection. I don’t want a diagnostic code to label someone. I don’t want to tell someone—or have someone else tell one of my patients—‘You have bipolar disorder’ or ‘You are depressed.’” Maybe they are, but there’s much more to it than that.”
The C Word
But what about cancer? Slow medicine is surely not adequate against it, right?
I ask that question, still a little skeptical that “slow” medicine can treat such an aggressive enemy. Dr. Finkelstein sees cancer patients often. It’s not that he doesn’t believe chemo and radiation can kill a tumor. But he goes back to the garden to explain: “Those conventional treatments are seeds you’re going to put into your body. They’re going to help if the soil is ready for them. You’ll just get better results.
“I want to be helpful to all my patients,” he says. “And that includes patients who are facing end-of-life issues. I sometimes encourage them to turn off the fight-or-flight mechanism and get into a slow rhythm. Restore balance. You’ll have a better quality of life if you are appreciating the present moment.”
That’s something he learned from Dr. Weil and has seen in his own practice ever since his secondary medical training. “Dr. Weil includes Western medicine in his approach,” he says. “But he also teaches that the patient should feel central to the process. The patient has got to feel in control.
“Trust is such an important factor in the doctor-patient relationship,” Dr. Finkelstein says. “I want patients to make decisions for themselves.” There are times when he needs to refer a patient to a specialist. He never gives just one name; he gives a slate of names and encourages patients to interview the doctors they’re considering.
Again, he returns to the garden. “Try different things,” he says of the search. “See what grows.” At the same time, he encourages patients to trust themselves—to be active participants in their care.
“I want to ease patients’ minds,” he continues. “I encourage people to slow down and recognize that the person staring back at them in the mirror each morning is the person who knows best. I want people to look at themselves and think: I am my own best doctor.”
First, Do No Harm
Perhaps the most important thing Dr. Finkelstein says during our 45-minute conversation is this: “Slow medicine as an approach is not harmful.”
There is no harm—no unwanted side effect—that can result from an integrative, holistic approach to wellness.
“I’m not selling anything,” he adds. “I’m not necessarily going to prescribe supplements. In fact, it’s more likely I’m going to recommend that you stop taking some of the supplements you’re on. I’m going to ask questions about them: Who prescribed them? What company manufactures them? What’s in them?
“I don’t want to tell anyone that what they’ve done is wrong,” he says. “But I will ask tough questions.”
Slow Progress for a New Approach
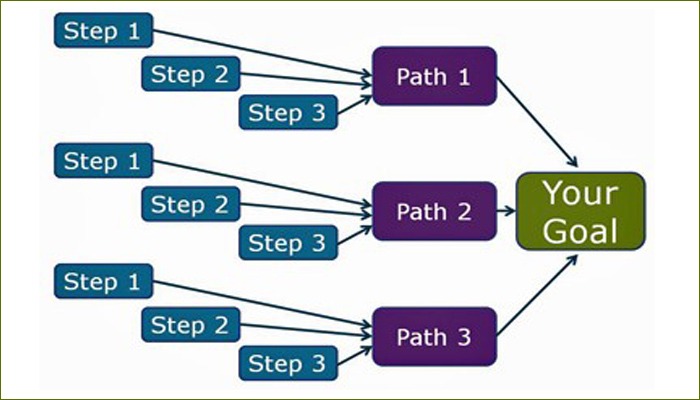
The slow-medicine approach— which Dr. Finkelstein thinks conventional medicine will eventually embrace—helps identify the root cause of our pain and then create a thoughtful, long-term response to addressing it. Slow medicine brings us back into balance.
Why does Dr. Finkelstein think it will take conventional medicine decades to accept the slow approach? “There is too great an alliance between the medical establishment and for-profit industry,” he says. “In medical school, I was bright-eyed and eager. I loved what I was learning, and I did well. Fifteen years into my practice, I realized the results fell far short of what I’d hoped. My patients weren’t having the outcomes I had expected. My own blood pressure was increasing. I developed an ulcer. I realized: if I were my own patient, I’d be giving myself medicine. But then I had to wonder, isn’t there something else I can do for myself?”
Slow medicine is to the health care industry (even that word connotes something massive and impersonal) what slow food is to the restaurant industry. If fast food is uniform, one-size-fits-all, large-scale-production dining, the slow food movement teaches us to appreciate where our food comes from and how it’s raised, to be curious about the farmers who raised it and to enjoy seasonal and often local ingredients.
RELATED: Combining Conventional & Integrative Medicine
Slow medicine doesn’t negate the need for surgery or other invasive treatment. But it does make our minds and bodies more fertile ground to accept such treatment.
Slow medicine allows us to be doctor/gardener hybrids—to be the compassionate caretakers of our own health.
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways