Physician Spotlight: Dr. Mark Wallace
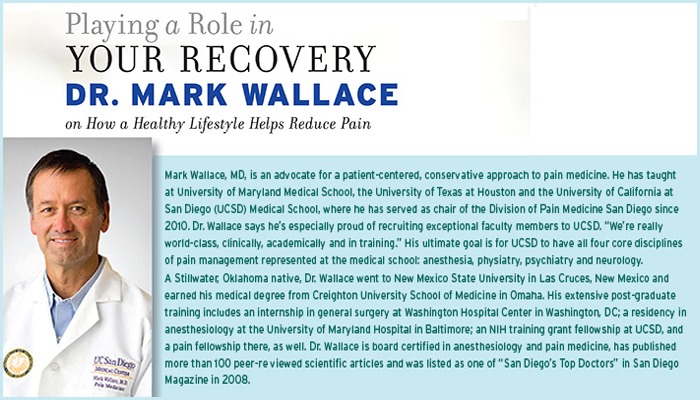
When Mark Wallace, MD, first greets a new patient, he asks two questions:
Not only does Dr. Wallace want to understand someone’s pain, he wants to know about the person in pain. And for him, the key is to uncover how well a patient has been taking care of himself. According to Dr. Wallace, there are few quick fixes. Instead of whipping out a prescription pad, Dr. Wallace challenges the person in pain to get on a path of wellness and share the responsibility for overall health. He asks patients to become partners in their health.
In his August 2012keynote address to incoming medical students at the University of California at San Diego (UCSD) he said, “I acquired the art of practicing medicine from my patients by observing them, listening to them and engaging them in the care I provided.”
The UCSD medical school professor and chair of the pain department went on to ask the audience, “So, what is the most conservative therapy?” Then he pro-vided the answer: “Teaching our patients the importance of healthy lifestyles. If we could get every patient in our society to live a healthy life by eating right, engaging in regular exercise and not smoking, to name a few … we would see a substantial decrease in heart disease, stroke, diabetes, chronic pain, mental disorders and even cancer.
“Your patients will listen to you,” he exhorted the future physicians. “They look up to you. A part of every visit should be education on the benefits of healthy living. If you can get your patients to engage in healthy lifestyles, then the therapies you initiate will be much more effective.”
Dr. Wallace advises his students: “Think simple and conservative first. Think of the least invasive treatment first …” It’s tough love for a society accustomed to a quick fix. While some physicians may jump to invasive treatments right away, Dr. Wallace thinks that’s a mistake.
And this doctor speaks from personal experience. Dr. Wallace lives with chronic pain himself and knows first hand the value healthy living has played in his rehabilitation. “I’ve had low back pain and a herniated disk in my neck,” he says. He’s had epidural steroid injections in his neck, but the real “trick” for him has been healthy living. “I do yoga and exercise regularly, I eat right and I get adequate sleep.” He tries not to take medication, but he will if he experiences a flare-up.
PUTTING AN INDIVIDUAL FIRST
At one time, Dr. Wallace wanted to be a surgeon. He found that he liked the OR, but felt it was “too focused on the interventional side.” He got into anesthesiology but missed working with patients who had chronic pain. “I wanted to engage long-term with patients,” he says. Twenty years ago, he decided pain medicine was the right discipline for him. “This is a challenging field,” he says of his chosen specialty. “You have to look at each patient individually. We can’t treat the masses. We treat individuals.”
Dr. Wallace is optimistic that he can help people, no matter what treatments they have tried. “I’ll dive right in,” he says of his approach. “I’ll revisit what they’ve tried before. It may be that they’ve already hit on something that works, but perhaps the dosage was inappropriate. Or maybe we should try a therapy they’ve used before in combination with another therapy.”
“I don’t want my patients to focus too much on what they’ve tried that hasn’t worked,” he says.
He looks at pharmacology, psychology and good old-fashioned healthy living as possible solutions to chronic pain, singly or in combination, and develops an appropriate treatment plan for each individual. “If I’m going to inject or medicate someone, it doesn’t start or end with that.
“A patient has got to take responsibility,” he says. “You can’t just be passive.”
FOUR PRIORITIES FOR TREATMENT EVALUATION
Dr. Wallace recommends four priorities when evaluating potential treatments.
• Efficacy
• Safety
• Ease of use
• Cost
“It is important that you consider the highest level of evidence when considering medical treatment efficacy,” he tells future doctors. “However, you must not let it blind you. What if it does not exist? In this case, I rely on clinical experience, which can be very powerful.
“Listen to your patients and observe their response to treatment,” Dr. Wallace offers. He believes you can learn a lot by listening.
As for safety, he suggests, “A therapy may have a very high level of efficacy based on clinical trials and clinical experience. However, there may be safety issues associated with the therapy. In this case, I may accept risks if the benefits are great. You have to discuss this with your patients and let them decide.” Again, the ideal patient is a partner.
NO THERAPY MAY BE THE BEST THERAPY
“The second scenario is a therapy that has no clinical trial data, but there is a vast amount of clinical experience with minimal safety issues,” he continues. “The last scenario is a therapy that has no clinical trial data, minimal clinical experience and significant safety concerns. In that case, you should either eliminate it or proceed very cautiously. Remember that no therapy is sometimes the best therapy. First do no harm.”
He says almost all his patients get completely well — or see significant improvement in their conditions—from living healthier lifestyles.
“Taking a pill each day is easier than going to a gym to exercise for an hour per day,” he says of his third priority. “It is easier than closely watching what we eat. Just because it is easy does not always make it the right thing to do.”
When he prescribes exercise, he advises starting slowly and gently: water aerobics or riding a recumbent bike, for example. Physical therapy may also be part of his recommendations, but it’s usually to jump-start a new plan. Physical therapy works well for acute pain, he says, but is less effective for chronic pain.
AGGRESSIVE TREATMENT FOR CANCER PAIN; BEING A SURVIVOR
The pain associated with terminal cancer is different, and Dr. Wallace says doctors must be aggressive in treating it.
He says cancer survivors dealing with pain need to be viewed differently from those who have terminal cancer. “We’ve been giving cancer survivors huge doses of opioids for pain, and they don’t need it,” he says of the way medicine has typically treated cancer pain. “We’ve got to say to these patients, ‘You are a survivor. I’m treating you for chronic pain now — not cancer pain.’”
He is wary of opioids. “They’re the only class of drug that grabs hold of a patient and won’t let go,” he says. “We’ve overused them because we don’t have alternatives.” Fortunately, he sees that changing. “In the future, I think we’ll have more targeted therapies that zero in on a specific area without all the side effects”of opioids.
THE FUTURE: NONTRADITIONAL THERAPY& THE VOICE OF PAIN MEDICINE
Dr. Wallace sees a healthy future in nontraditional therapies. He and his team collaborate often with the Center for Integrative Medicine at UCSD — not as a single modality, he says, but as part of a greater whole. According to Dr. Wallace, patients are “amazingly open” to nontraditional therapies. The challenge is that insurance companies may be reticent to cover them.
A final challenge Dr. Wallace sees in his field: Who’s the official voice of pain medicine? He doesn’t feel there currently is one. “There are too many different societies and academies,” he says. “And they’re not necessarily working together. “When someone asks me who the official voice of pain management is, I have to say, ‘I don’t know.’ Other fields of medicine aren’t like that. I don’t know the answer, but I do know we’ve got to stop working in isolation.”
It’s all about balance, Dr. Wallace believes — between risk and reward, cost and benefit and interventional treatments and healthy living. {PP}
PainPathways Magazine
PainPathways is the first, only and ultimate pain magazine. First published in spring 2008, PainPathways is the culmination of the vision of Richard L. Rauck, MD, to provide a shared resource for people living with and caring for others in pain. This quarterly resource not only provides in-depth information on current treatments, therapies and research studies but also connects people who live with pain, both personally and professionally.
View All By PainPathways